Cancer is usually described as a disease of mutations. Genes break, pathways fail, and cells escape control. That framing has been powerful, but it misses a deeper layer that may reveal how it begins.
The human genome is not primarily a coding genome. It is a repeat genome. More than half of our DNA consists of repetitive elements, with Alu retroelements alone numbering over a million copies. These sequences are a defining feature of primate genomes and they create a unique biological problem that human cells must continuously manage. Recent work suggests that cancer may emerge, in part, when this management system loses balance.
Alu elements are short retrotransposons that readily form double‑stranded RNA stem‑loop structures when transcribed, particularly in antisense orientation within introns and untranslated regions. To the innate immune system, these structures resemble viral RNA. This means that normal gene expression in human cells constantly risks triggering antiviral immune responses against self‑derived RNA.
A striking recent study shows that human cells rely on active suppression to avoid this outcome. In Ku suppresses RNA‑mediated innate immune responses in human cells to accommodate primate‑specific Alu expansion, the authors demonstrate that the DNA repair protein Ku (Ku70/Ku80) plays an essential second role: binding Alu‑derived dsRNA stem‑loops and preventing activation of innate immune sensors such as MDA5, RIG‑I, PKR, and OAS/RNase L.
When Ku is depleted interferon and NF‑κB signaling are strongly activated, translation is suppressed, and cells undergo growth arrest or death. Notably, Ku levels scale tightly with Alu expansion across primates, and Ku is essential in human cells but not in mice. The implication is clear:
Human cell viability depends on continuous suppression of Alu‑derived innate immune activation.
Alu expression is not harmless noise, it is actively tolerated! Ku functions as a finite buffer that allows primate cells to tolerate structurally immunogenic RNA produced by repeat‑rich genomes. When structured RNA load increases simultaneously from endogenous repeat transcription and exogenous viral RNA infection, Ku becomes functionally saturated and redistributed, weakening nuclear retention and cytoplasmic buffering. This pressurizes the cell’s capacity to contain dsRNA stress, promoting escape of repeat‑derived RNA, activation of innate sensors, and eventual selection for immune‑tolerant states.
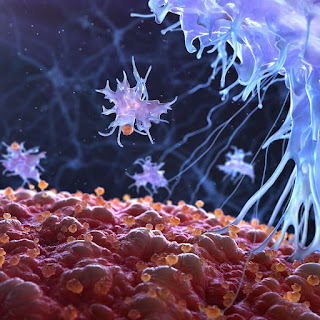
A second line of evidence connects this tolerance to cancer evolution. A 2025 bioRxiv preprint, p53 loss promotes chronic viral mimicry and immune tolerance, shows that loss of p53 permits transcription of immunogenic repetitive elements, generating signals that resemble viral infection. Rather than leading to effective immune clearance, this state becomes chronic. Tumor cells adapt by dampening innate immune responses and tolerating persistent repeat‑derived nucleic acids.
In this view, “viral mimicry” is not a one‑time immune alarm. It is a conditioning process repeat RNAs accumulate, immune pathways are activated, and progressively suppressed or rewired to allow survival. Cancer cells do not simply evade immunity, they learn to live with endogenous viral‑like signals.
These immune findings align with earlier evidence that repeat control begins at the level of genome structure itself. A 2022 Nature Communications study demonstrated that retroelements embedded within the first intron of TP53 act as cis‑repressive genomic architecture. Removing this intron increases TP53 expression, indicating that long‑embedded repeats contribute directly to regulating a core tumor suppressor gene.
Importantly, this repression is architectural rather than motif‑driven. The repeats do not act through a single conserved sequence, but through repeat‑dense structure.
Together, these findings suggest a layered system of control:
Structural repression of repeats within introns.
Immune suppression of repeat‑derived dsRNA.
p53‑dependent governance of both genome stability and immune signaling.
One long‑standing challenge in repeat biology is inconsistency. Different tumors show different repeat fragments. Even different regions of the same tumor can look unrelated at the sequence level.
From a traditional biomarker perspective, this appears discouraging. From a structural perspective, it is expected. Codondex analyses of repeat‑dense introns, including TP53 intron 1, show that cancer does not preserve specific Alu sequences. Instead, it perturbs repeat topology:
dominance and skew within intronic scaffolds,
stem‑loop‑prone architectures,
context‑specific fragmentation patterns.
The sequences vary. The instability regime does not. This is characteristic of a state change, not a discrete genetic event. Repeat‑dense introns behave like stress recorders. They integrate replication stress, chromatin relaxation, repair pathway bias, and immune tolerance history.
Unlike coding mutations, these signals are heterogeneous, region‑specific, and reflective of ongoing cellular state.
They are difficult to interpret with gene‑centric tools, but powerful when viewed architecturally.
Most cancer diagnostics ask:
What mutation is present? A repeat‑aware framework asks:
Has this tissue entered a stable state of repeat derepression coupled with immune tolerance?
That state may precede aggressive behavior, accompany treatment resistance, or mark transitions in disease evolution. Future prognostic approaches may therefore combine repeat‑topology instability metrics, repeat RNA burden, and evidence of immune decoupling from dsRNA load. Not to identify a single driver, but to detect loss of containment.
Alu repeats do not cause cancer on their own, but human cells must continuously restrain them, structurally and immunologically. Cancer appears, at least in part, when that restraint erodes and tolerance replaces control. Introns, long treated as background, may be one of the clearest places to see this shift, not because they encode instructions, but because they actively record genomic history and project it into a measure of present state.